News and Highlights
Current Features: High Praise ♦ Career Awardee ♦ High Impact Work
Previous Features: Archive
Note concerning links to non-VA websites: The VA does not endorse and is not responsible for information, products, or services at non-VA websites.The Incomparable Dr. Rose
 Note: This article includes excerpts from stories posted by the University of Florida (here) and Brooks Rehabilitation (here and here).
Note: This article includes excerpts from stories posted by the University of Florida (here) and Brooks Rehabilitation (here and here). Dorian K. Rose, PhD, (pictured at right working with a patient) is exceptional as a person let alone as a neurorehabilitation researcher in light of her gratitude to persons who have helped her throughout her career as well as the numerous awards she has received. Dr. Rose’s latest honor is being named a Catherine Worthingham Fellow by the American Physical Therapy Association (APTA), which recognizes professional excellence and serves as an inspiration to other physical therapists (PTs). This honor is given to PT members who have demonstrated unwavering efforts to advance the PT profession for more than 15 years.
“Receiving this honor and being recognized for doing what I have the privilege and opportunity to do every day is humbling and fills me with gratitude for both those who have gone before me and my current colleagues and clients,” said Dr. Rose.
She also noted, “Professional development takes a village and I have been fortunate to have had committed mentors and strong teams to work with at the Malcom Randall VA, the University of Florida, and Brooks Rehabilitation.”
With a PhD in Biokinesiology from the University of Southern California (2004), Dr. Rose joined the BRRC in 2010 with a 5-yr Career Development 1 Award from the VA Rehabilitation Research & Development Service (RR&D) to study combining neural and behavioral therapies to enhance stroke recovery. This was immediately followed by an RR&D Career Development 2 Award, also 5 years, to study a novel strategy to prevent falls after stroke. The purpose of this research was to test backward walking as a way to improve gait speed and balance. At the same time as the 2nd award, Dr. Rose received an additional 2-year RR&D grant, to study whether biofeedback combined with verbal feedback from a therapist would improve walking after a stroke. The results of this work have often been significant and provided data on how to improve mobility after a stroke that impairs walking or even upper extremity abilities.
Another significant feature of Dr. Rose’s work is her ability to collaborate – her research has always included collaboration with Brooks Rehabilitation in Jacksonville, Florida, and the University of Florida.
Here are some inspiring and thought-provoking excerpts (updated) from a 2022 interview with Dr. Rose conducted at Brooks Rehabilitation, where she discusses the importance of research that is focused on improving the lives of patients (with picture below at right showing Dr. Rose working with a recent patient):

I make sure that the questions I ask or the grants I propose have a clinical component to them. My goal is to always design questions that can impact the care that patients receive. That has to always be in the forefront of my mind. For example, the notion of backward walking post-stroke originated from hearing physical therapists describe their experiences in the clinic and hearing patients in those clinics describing their struggles. I need to make sure I’m always bringing it back to the patient. That’s what’s critical.
We’ve been studying backward walking for about 8 years and learning more about the role it can play in recovery, but there are always additional questions to explore – we keep peeling the onion. In a previous study, we examined the effectiveness of a novel Backward Walking Training Program to improve walking speed and balance immediately after stroke and later in stroke recovery. Results from the study showed that the backward walking improved walking speed and balance confidence more than the standard balance training program. A new area of inquiry for our research team is how is our walking training program affecting the brain itself. As a physical therapist, I have learned that performing challenging tasks and learning new motor skills can indeed change pathways in our brain. In our newest study, we use functional magnetic resonance imagining (fMRI) to visualize the brains of our post-stroke patients and ask two questions:
- Before the backward walking program is started, what does brain activity look like and does that predict how a patient will respond to the intervention?
- After the backward walking program, will we see changes in the brain related to walking and balance ability?
A full list of research articles authored or coauthored by Dr. Rose is available at this National Library of Medicine link.
Note that two other previous BRRC PT researchers were also recognized with the Worthingham Fellowship:
- Andrea Behrman, PhD, PT, FAPTA – 2009 Fellow (BRRC from 1999 to 2010)
- Carolyn Patten, PhD, PT, FAPTA – 2016 Fellow (BRRC from 2007-2018
Building Knowledge through Mentoring
New blood can be literally life-saving for persons with certain medical conditions, for example trauma, but it is also a metaphor referring to the benefit a new person can bring to an organization or a project. That is a particularly apt metaphor for an up and coming professional brought into an organization who is filled with new, innovative ideas and dynamic energy that fuel discovery. Therefore, the VA wisely established a Career Development Program to enable junior researchers to be mentored by renowned and experienced VA researchers. Indeed, several BRRC Career Development awardees (CDAs) have become recognized for their work, for example, David J. Clark, PhD, and Dorian K. Rose, PhD. One of the newer CDA researchers at the BRRC is Dana Otzel, PhD, a Florida native from Ocala. Dr. Otzel’s research involves highly technical laboratory work that focuses on evaluating neuromuscular deficits and locomotor recovery after spinal cord injury (SCI). She is currently examining the role of hormone therapy for musculoskeletal problems caused by SCI. She started with the VA at the Geriatric Research, Education, and Clinical Center (GRECC) with a fellowship and then came to the BRRC as a CDA-1 under the mentorship of BRRC investigators, Drs. Yarrow and Clark, and GRECC investigator Dr. Borst.
One of the newer CDA researchers at the BRRC is Dana Otzel, PhD, a Florida native from Ocala. Dr. Otzel’s research involves highly technical laboratory work that focuses on evaluating neuromuscular deficits and locomotor recovery after spinal cord injury (SCI). She is currently examining the role of hormone therapy for musculoskeletal problems caused by SCI. She started with the VA at the Geriatric Research, Education, and Clinical Center (GRECC) with a fellowship and then came to the BRRC as a CDA-1 under the mentorship of BRRC investigators, Drs. Yarrow and Clark, and GRECC investigator Dr. Borst. Her CDA-1 led to her current CDA-2 award to study the effect of an enzyme that has a key effect of converting testosterone to estrogen. She is examining the effect this enzyme has on neuromuscular plasticity when testosterone is combined with locomotor training for SCI rehabilitation. As more is learned about the neural system and neuroplasticity, it becomes clearer that biochemistry and physical therapy are linked. Dr. Otzel's CDA-2 mentors are Drs. Yarrow and Bose of the BRRC and Dr. Barton of the University of Florida.
Dr. Otzel noted about her work, “I have enjoyed the journey of being able to conduct research in the clinical SCI population and expanding into a new direction of preclinical research. This transition is attributable to the strong mentorship that I’ve had.”
The following two articles first authored or co-authored by Dr. Otzel have received recognition:
 Otzel DM, Kok HJ, Graham ZA, Barton ER, Yarrow JF. Pharmacologic approaches to prevent skeletal muscle atrophy after spinal cord injury. Curr Opin Pharmacol. 2021 Oct;60:193-199.
Otzel DM, Kok HJ, Graham ZA, Barton ER, Yarrow JF. Pharmacologic approaches to prevent skeletal muscle atrophy after spinal cord injury. Curr Opin Pharmacol. 2021 Oct;60:193-199.Current Opinion in Pharmacology invites authors who are considered leaders in their fields to write review on recent developments in their fields. Thus, Dr. Otzel at an early point in her career is already being recognized for her expertise.
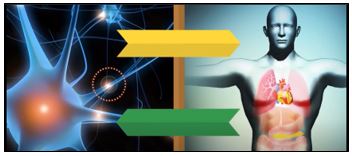
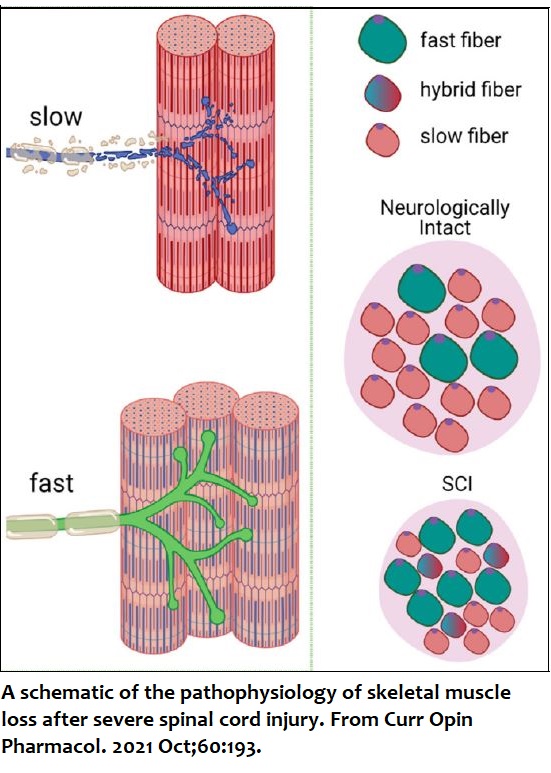
One aspect of SCI discussed in this article is a cascade of events: SCI impairs neural drive. This in turn causes motor neurons to atrophy. This then leads to pathological changes in the neuromuscular junction. These effects combine to decrease muscle force and/or to cause paralysis (see figure at right; generated in BioRender). Collectively, these deficits impact the rapid rate of muscle atrophy and the repeated denervation–reinnervation cycles that influence the muscle fiber-type transition (from slow-oxidative to fast-glycolytic) in paralyzed muscles.
The authors concluded that compounds that target "molecular signatures" in atrophic muscle after SCI appear to hold the greatest potential to lessen muscle loss and/or to promote muscle recovery, especially when combined with established activity-based physical therapies that "reload" the paralyzed limbs. The full text of the article is available at this link.
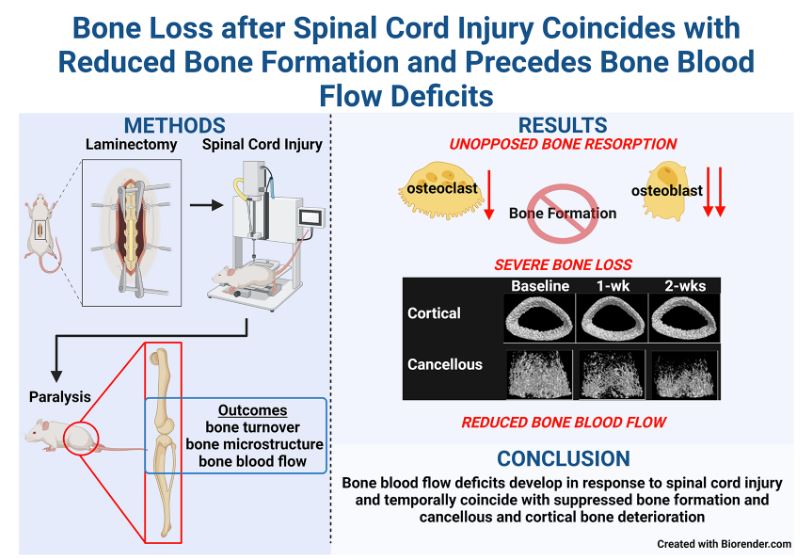
 Yarrow JF, Wnek RD, Conover CF, Reynolds MC, Buckley KH, Kura JR, Sutor T, Otzel DM, et al. Bone loss after severe spinal cord injury coincides with reduced blood formation and precedes bone blood flow deficits. J Appl Physiol. 2021;131(4):1288-1299.
Yarrow JF, Wnek RD, Conover CF, Reynolds MC, Buckley KH, Kura JR, Sutor T, Otzel DM, et al. Bone loss after severe spinal cord injury coincides with reduced blood formation and precedes bone blood flow deficits. J Appl Physiol. 2021;131(4):1288-1299.A figure from this article was chosen by the journal for the Spotlight Cover of the issue in which the article was published (see journal cover at right) The Journal of Applied Physiology is a highly regarded journal that published its first issue in 1948.
Below is a graphical abstract of the article that illustrates the main aspects of the work. Graphical abstracts are designed to help a reader quickly gain an overview of the research described in an article and determine whether it is relevant to the reader’s own research. The full article is available at this link.
A complete list of Dr. Otzel's publications can be accessed at this link. Back to Top
BRRC Article Has High Impact in Neuroscience
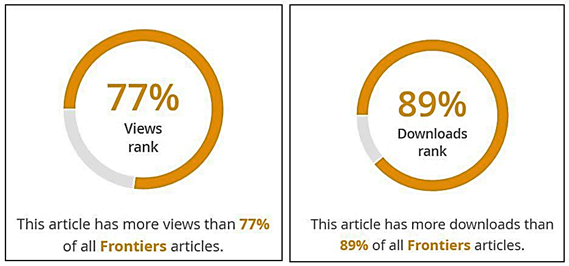 The following article published by a BRRC team and collaborators was selected as one of the top motor neuroscience articles published by the Frontiers in Human Science in 2021 (BRRC authors in bold italic):
The following article published by a BRRC team and collaborators was selected as one of the top motor neuroscience articles published by the Frontiers in Human Science in 2021 (BRRC authors in bold italic):
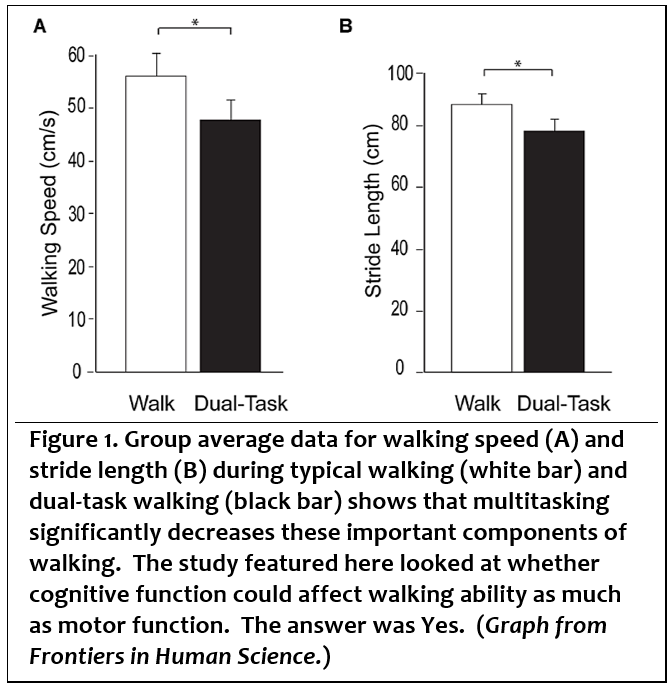
The article reported on BRRC research showing that, after a stroke, recovery of the ability to walk is explained in part by task-related activity in frontal regions of the brain that control cognitive functions. Recovery of walking function can be affected by cognitive function as well as motor function.
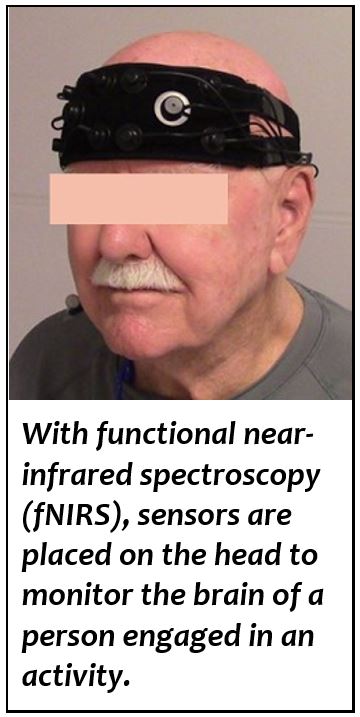
The ability to walk is a significant contributor to quality of life, and this study shows that there are many factors that must be considered to plan the most effective rehabilitation interventions. The advances made by this work are possible through the use of functional near infrared spectroscopy (fNIRS). This emerging technology allows for recording of brain activity even while a person is performing movement tasks such as walking.
Dr. Clark explained: “fNIRS technology has opened a new field of rehabilitation research, because we can now assess how real-time activity in the brain is related to walking task performance. Brain activity recorded with NIRS will be a crucial outcome measure in future rehabilitation trials.” In this study, activity was recorded from only a small region of the brain, but other regions are also involved in control of walking and could be examined by future studies.
The BRRC scientists who conducted the research are specialists in biomechanis, biokinesiology, physical therapy, neurology, and aging:
- Sudeshna Chatterjee, PhD, the first author of the article, had been a doctoral student and postdoctoral researcher with the BRRC at the time the work was done and was mentored by coauthors, David J. Clark, ScD, and Dorian K. Rose, PhD. She is now an Assistant Professor at Drexel University in Philadelphia.
- Dr. Clark and Dr. Rose co-lead the Motor Function Initiative of the Brain Rehabilitation Research Center and, as previously reported here, have both been honored by prestigious awards: Dr. Clark received the PECASE award and Dr. Rose has received numerous awards from professional organizations.
- Janis J. Daly, PhD, was the Director of the BRRC from 2011 to 2019.
- Dana M. Otzel, PhD, is a current Career Development 2 scientist whose work is focused on the effect on neuromuscular plasticity of testosterone combined with locomotor training after spinal cord injury.
Frontiers collects at least ten articles by topic from all the articles published every 2 years in the journal; the collections are called Frontiers in Research Topics. With their unique mix of varied contributions from Original Research to Review Articles, Research Topics unifies the most influential researchers and the latest key findings and historical advances in hot research areas.
A list of articles based on collaborations among BRRC investigators over time is available at this link.
Archive
Schiefer - Top 100 Article ♦ Award-Winning PT Rose ♦ Schiefer on Codeathon Grand Prize Team
Williamson and Lamb Explore TBI ♦ Schiefer Neuromodulation ♦ Clark Presidential Award
Rose and Golden Synapse ♦ Waid-Ebbs and TBI
Schiefer and Team Article on Stomach Neural Signals and Diet
Has Double Significance
Articles reporting research results are critical to the progress of scientific knowledge. In many cases, these articles have a small impact on science. Together, however, these small impacts are critical to the foundation of science. Occasionally, a single study itself can have a major impact. Some new method, results, or hypothesis can represent a very big step forward.
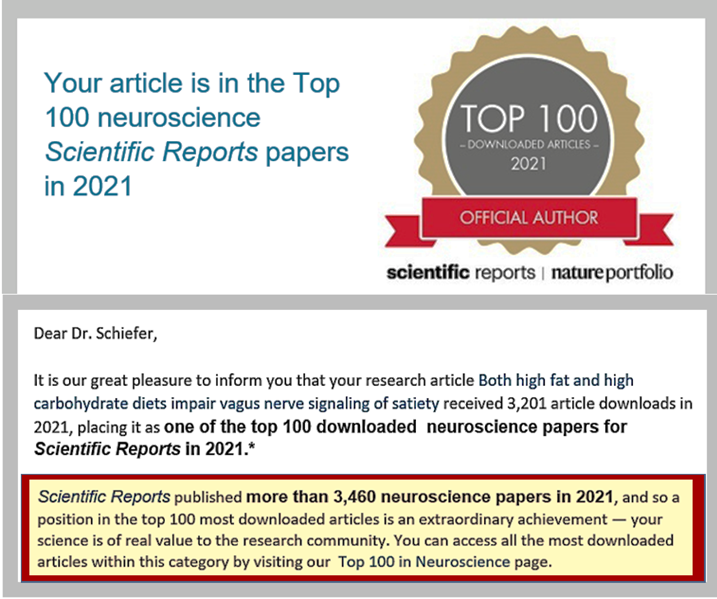
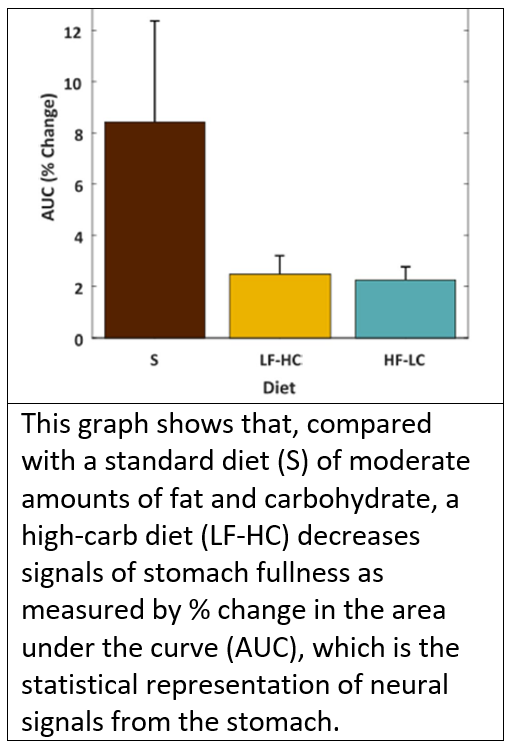
A 2021 paper* on a study conducted by a team led by BRRC investigator, Matthew A. Schiefer, PhD, has proved to be a paper that is having a major impact as indicated by how often it has been downloaded from the journal by other scientists. This paper reported on both a new method and important new results:
- The new method uses established technology in a new way. An array of recording electrodes typically used in the brain is, instead, inserted into a nerve in the neck, which makes it unnecessary to sever the nerve. Dr. Schiefer and team showed that the array could detect stomach signals, specifically the signals associated with fullness. Compared with severing the nerve, inserting the array in the nerve is less damaging to the nerve while still affording a high fidelity (accuracy in electrical signal).
- The new result is that, similar to a high-fat diet, a high-carbohydrate diet can also decrease the neural signals from the stomach indicating that the stomach is full. The consequence is that, following long-term consumption of high-fat or high-carbohydrate diets, more food is required for the stomach to generate a full signal. This dysfunction has the potential to promote overeating and obesity.
Although Dr. Schiefer is listed as the last author, this does not mean he did the least. Far from it. In a science publication tradition, the author who provided guidance to other persons assisting with the study is often listed as the last author, also known as “senior” author. Indeed, in this case, according to a section titled “Author Contributions” at the end of the paper, although all authors wrote or revised one or more sections of the paper, Dr. Schiefer also had trained 4 of the other authors on how to conduct the study; he conducted experiments and acquired data himself; and, after his own training on analysis of this particular type of data from one of the other authors, he also analyzed the data. The others on Dr. Schiefer’s team were: Hailley Loper, BS and Logan Bassoff, BS, who were VA staff affiliated with the University of Florida; Jack Sample, MD a general surgery resident at Mayo Clinic in Rochester, MN who conducted research in Dr. Schiefer’s lab at the Louis Stokes VA Medical Center in Cleveland, OH; and Monique Leinen, BS, who is currently a research technician with the BRRC.
I decided to transition to neuromodulation of the autonomic nervous system, which is the part of the nervous system that controls most of the things that we don’t think about. I decided to focus there because obesity is such a big problem. High blood pressure is also a big problem, so I am also working to develop closed-loop, bi-directional control of arterial blood pressure by modulating the activity in the greater splanchnic nerve.
The complete paper is available here at PubMed Central: Both high fat and high carbohydrate diets impair vagus nerve signaling of satiety. A complete list of Dr. Schiefer’s publications is available at this link.
Rose’s Award-Winning Work Advances Physical Therapy

Dorian K. Rose, PhD (image right from MedBridge), has received another award – approximately her 9th: The Lucy Blair Service Award from the American Physical Therapy Association (APTA). The award honors APTA physical therapists “whose contributions to APTA are of exceptional quality.”
“Exceptional quality” is a perfect description of Dr. Rose. On receiving her PhD in 2004 from the University of Southern California, she received an award that recognizes leadership potential. She came to the BRRC in 2010 as a Career Development 2 grantee and, since then, her work has been consistently awarded or recognized for its contribution to the field of physical therapy as a part of neurorehabilitation – see list below.
As noted by a colleague of Dr. Rose who wrote a letter in support of the nomination of Dr. Rose for the Lucy Blair Service Award: “Collaborating with someone like Dorian, who cares deeply about the project [and] is hard-working and selfless made the work fulfilling and ultimately, a great success.”
The BRRC is lucky and proud to have Dr. Rose as one of its scientists. Congratulations to Dr. Rose for another award – and a thank you for being exceptional!
Awards recognizing work by Dr. Rose and articles she coauthored: 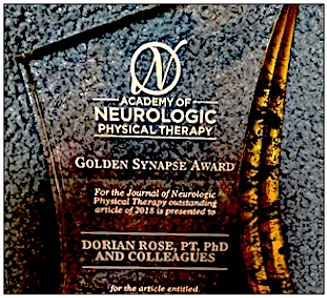
- 2020 Lucy Blair Service Award, American Physical Therapy Association (APTA).
- 2018 Golden Synapse Award from the Academy of Neurologic Physical Therapy (right).
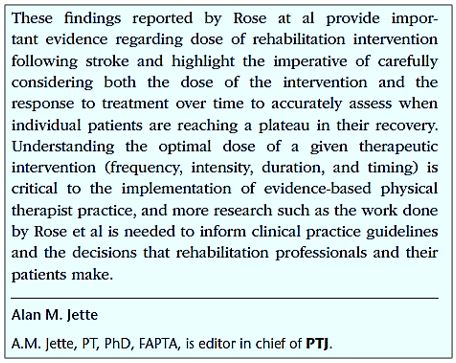
- 2017 article by Rose and her team in the journal, Physical Therapy Journal (PTJ) accompanied by an editorial noting its importance (see excerpt below right). Also received University of Florida Dean’s Citation Paper Award.†
- 2012-2011: Two awards noted significance of an article coauthored by Dr. Rose‡: 2012 Stroke Progress and Innovation Award from the American Heart Association.
- 2011 Dorothy Briggs Memorial Scientific Inquiry Award.
- 2010 J. Brooks Brown Annual Research Award, Brooks Rehabilitation Center.
- 2010 APTA Neurology Section: Service to the Section Award.
- 2009 Early Career Poster Award. American Congress of Rehabilitation Medicine/American Society of Neurorehabilitation.
- 2004 Golden Cane Award Department of Biokinesiology and Physical Therapy University of Southern California.
* Rose DK, DeMark L, Fox EJ, Clark DJ, Wludyka P. A backward walking training program to improve balance and mobility in acute stroke: A pilot randomized controlled trial. Journal of Neurologic Physical Therapy. 2018 Jan;42(1):12-21.
† Rose DK, Nadeau SE, Wu SS, Tilson JK, Dobkin BH, Pei Q, Duncan PW. Locomotor training and strength and balance exercises for walking recovery after stroke: response to number of training sessions. Physical Therapy. 2017 Nov 1;97(11):1066-1074. Excerpt at right.
‡ Tilson JK, Sullivan KJ, Cen SY, Rose DK, Koradia C, Azen SP, Duncan PW. Meaningful gait speed improvement during the first 60 days post-stroke: minimal clinically important difference. Physical Therapy. 2010; 90[2]:196-208.
A list of Rose’s research publications and in some cases full texts are available at this National Library of Medicine link. (Return to Archive list or Top)
Schiefer and Team Win Grand Prize for Creating a Program to Make Bioelectronic Research Data More Accessible and Usable
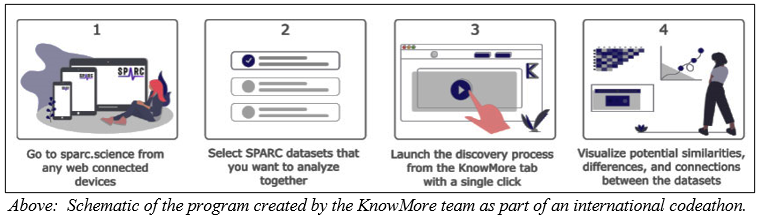
Matthew A. Schiefer, PhD, competed as a team member in the international 2021 SPARC FAIR Codeathon, and he and his team won a Grand Prize that included a $20,000 cash award.
- What is a codeathon? It is a combination of the words coding and marathon, so in other words, it was a race to come up with the best computer program, which is created with coding.
- What is SPARC? SPARC, or Stimulating Peripheral Activity to Relieve Conditions, is a program funded by the National Institutes of Health (NIH) with the goal of transforming our understanding of nerve-organ interactions in order to advance bioelectronic medicine and to discover bioelectronic treatments that can change lives. The history of this field of medicine was detailed by Time magazine, which noted that SPARC “aims to map out every nerve of the human nervous system outside the brain. That could illuminate new ways to manipulate electrical signals to control cells.” There are also videos that explain more about this field of medicine at this NIH webpage.
- What is FAIR? It is the name of a scientific initiative based on the words Findability, Accessibility, Interoperability, and Reuse. This initiative is attempting to address problems resulting from how people, especially scientists, increasingly rely on computer programs to deal with data as a result of the increase in volume and complexity of data and the speed at which new data are created.
Dr. Schiefer was one of about 25 competitors chosen to participate in the virtual codeathon out of competitors who applied from all over the world. SPARC then created small teams, each with various backgrounds and expertise, and provided an experienced leader for each team. In Dr. Schiefer’s case, this resulted in the following 4 team members, who called themselves the KnowMore Team:
- Bhavesh Patel (Lead), is from California Medical Innovations Institute in San Diego.
- Matthew A. Schiefer (Writer - Manuscript), a VA Career Development Scientist, joined the BRRC in Gainesville, Florida, in 2018.
- Ryan Quey (SysAdmin), a consultant with Anant Corporation currently living in Cambodia.
- Anmol Kiran (Writer - Documentation), with the Institute of Infection, Veterinary & Ecological Sciences in Liverpool, United Kingdom, is currently living in Malawi.
A team of judges from the NIH was given the difficult task of judging the codeathon projects based on the criteria of creativity, impact on SPARC users, feasibility, and completeness of documentation. The KnowMore Team won by creating a program that allows a user to pull data from a multitude of SPARC research datasets and to run analyses that can provide:
- A series of graphs that quickly allow the user to visually compare data across multiple studies, which was Dr. Schiefer’s primary contribution.
- A table comparing the types and amount of data collected in the different sets of data.
- A special map (heat map) of how well correlated the data are (a confusion matrix) based on words used in the data set.
- An abstract of the studies.
- A description of the relationships between the investigators, institutions, and funding sources of those who created the data.
- A wordle, or graphic image similar to a logo but composed of just words, that represents the data.
Dr. Schiefer has used functional electrical stimulation [FES] for neuromodulation to treat a variety of health problems. FES involves using a very low electrical current to stimulate nerves. He described his work with FES as follows:

My current research is looking at how to use FES to stimulate specific autonomic nerves to treat obesity (vagus nerves) and control blood pressure (splanchnic nerves). Both conditions affect many Veterans as well as the general population. My long-term goal is to develop implants that contain “smart systems” that stimulate the nerves to treat these conditions. Several SPARC studies involve this type of work. The data from those studies are uploaded to the SPARC system to enable scientists to learn from each other. These data could be quite relevant for my research. Participating in the codeathon gave me insight into how the data are stored and how the data can be used. I also saw how inconsistencies between data sets make it difficult to see the big picture, and my team worked on a way to solve that problem.
In support of Dr. Schiefer’s work, the VA will be funding the following research grant proposal he submitted: Developing a Novel Stimulus Paradigm and Interface of Vagal Nerve Stimulation (VNS) to Treat Obesity. Normally grants must be resubmitted several times before they are approved, but this proposal was funded on its first submission, which is evidence of the importance of the work and of Dr. Schiefer’s research ability.
A list of Dr. Schiefer’s publications is available at this link. (Return to Archive list or Top)
Sleep and Posttraumatic Stress Disorder (PTSD): An Autonomic Pathway to Treatment for Veterans with Traumatic Brain Inury (TBI)
The autonomic functions most people know of are breathing and the beating of the heart. John B. Williamson, PhD, has long focused his research on the autonomic system (ANS), which is actually involved in every essential human function including emotion and sleep. It is the involvement of the ANS in emotion and sleep problems that Dr. Williamson is currently exploring. Such problems often occur with psychiatric disorders – including PTSD – and can cause problems that are insidious such as deterioration in health and thinking. Indeed, a recent study at a single VA medical center documented that, of post 9-11 Veterans who were likely to have an alarmingly high rate of insomnia, for Veterans with PTSD, the rate of insomnia was 93% compared with 30% in the general population. Developing an effective treatment requires a better understanding of what underlies both sleep disorders and emotional dysfunction.
In 2013, Williamson, working with BRRC Career Development scientist, Damon G. Lamb, PhD, and others, published a paper on a theory of how disruption of the ANS could cause symptoms of posttraumatic stress disorder (PTSD) in persons with traumatic brain injury (TBI): Symptoms such as anger and increased vigilance (alert watchfulness for danger) as well as flashbacks and nightmares may result from “altered ANS activity in response to psychological and physical challenges.” Further, “TBI induced damage to networks that regulate the ANS increase vulnerability to PTSD.”
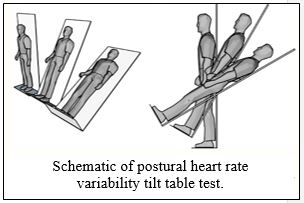
When the effect of tVNS on symptoms of PTSD was tested, results were positive—the autonomic response of the Veterans to startle decreased. Developing this work further, Williamson as principal investigator with Lamb and Porges as coinvestigators are beginning a 4-year study funded by VA Rehabilitation Research and Development Service. The study will explore the use of tVNS as a treatment for sleep problems for Veterans with PTSD alone and those with both PTSD and mild TBI.
Aside from the ability to decrease emotional reactivity, tVNS is both non-invasive and simple. The stimulation is applied externally to the ear. If effective, by alleviating sleep problems, this treatment may improve participation in daily activities, which can be seriously hampered by PTSD symptoms. Data from this study may also help with another challenge that remains even for treatments that appear to be simple, in this case: how much stimulation should be used and how often.
Both Williamson and Lamb joined the BRRC as Career Development 2 scientists, Williamson in 2012 and Lamb in 2018.
Lists of Williamson’s and Lamb’s research publications, and in some cases full texts, available at these National Library of Medicine links: Williamson and Lamb. (Return to Archive list or Top)
Schiefer Invited by National Institutes of Health (NIH) to Contribute to Exploration of Bioelectronic Medicine

Matthew A. Schiefer, PhD, came to the BRRC from Case Western Reserve University and the Louis Stokes VA Medical Center in Cleveland in the midst of working on a VA Career Development Award (CDA)-2. One of his projects completed in Cleveland was featured in Research Currents, which is published by the VA. In that project, he worked on a way to make a hand prosthetic provide a sense of touch (right), which provides critical information on factors such as pressure, pain, temperature, and movement, all needed for safety and function. At the BRRC, Schiefer will gain new expertise and skills in bioelectronic research that will make him one of the few VA scientists to have such expertise and will put him on the cutting edge of neuroscience and biomedical engineering.
In keeping with this work, Schiefer applied for a highly competitive opportunity to be part of a special program at the NIH: The Stimulating Peripheral Activity to Relieve Conditions program (SPARC). This program is providing opportunities and funding to advance research on bioelectronic medicine and the therapeutic use of neuromodulation. A well-established form of this treatment that many people know about is the implantable cardiodefibrillator (ICD), which is used to prevent irregular heartbeats. The history of this field of medicine was recently detailed in Time magazine, which noted that SPARC, “aims to map out every nerve of the human nervous system outside the brain. That could illuminate new ways to manipulate electrical signals to control cells.”
With his strong background in bioelectronic medicine, Schiefer was 1 of only 30 nationwide selected to attend the Predictive Modeling to Inform Development of Bioelectronic Medicine Therapies meeting. The meeting consisted of an interactive experience bringing together diverse interdisciplinary teams to tackle the challenge of simulations of bioelectronic medicine approaches for diseases and conditions that impact the stomach (ulcers), the colon (irritable bowel syndrome), lungs (asthma), heart (irregular heartbeat), or lower urinary tract (chronic urinary tract infections).
Dr. Schiefer noted: “I had to submit an application that contained, among other things, projects that I want to work on, how I think I can help shape the field going forward, and where I see the field in the future. . . . The workshop was conducted virtually over the course of a week. At the conclusion of the course, I had developed collaborative grants with researchers at Purdue University and the University of Pittsburgh.”
How does this work relate to brain rehabilitation? Schiefer was just awarded a VA grant to pursue research on closed-loop control of homeostatic blood pressure following spinal cord injury (SCI). Chronic low blood pressure can be a serious problem after SCI, and the type of research Schiefer is pursuing shows promise.
More information about Schiefer and a list of his publications is at this link. (Return to Archive list or Top)
Clark Receives National Presidential Award
 Above: Dr. Clark with his wife at the ceremony. Lower right: The award was celebrated by the Chief Research and Development Officer, Rachel B. Ramoni, DMD, ScD, with cake.
Above: Dr. Clark with his wife at the ceremony. Lower right: The award was celebrated by the Chief Research and Development Officer, Rachel B. Ramoni, DMD, ScD, with cake.
David J. Clark, ScD (shown above with his wife at the award ceremony), received the highest honor bestowed by the U.S. to outstanding independent early-career scientists and engineers: The Presidential Early Career Award for Scientists and Engineers (PECASE). This annual award
recognizes contributions to the advancement of science, technology, education, and mathematics (STEM) as demonstrated by scientific leadership, public education, and community outreach. Clark was 1 of only 4 scientists from the VA who were selected. Clark received the award at a ceremony held at Constitution Hall in Washington DC.
Clark explores neural control and rehabilitation of walking affected by neurologic impairments, particularly those that affect the frail elderly and those caused by stroke. By conducting clinical trials of walking rehabilitation and motor learning, Clark obtains data on the role the central nervous system plays in walking so he can then improve treatments to restore functions that impact walking such as balance and speed. In his current research, Clark uses brain neuroimaging methods such as functional near-infrared spectroscopy (fNIRS) to measure activity in the cortex of the brain during walking. To augment learning and functional recovery, he also uses painless, noninvasive electrical stimulation techniques with research participants while they practice complex walking tasks.
Clark has been with the BRRC since 2007, when he received a Career Development 1 Award from the Rehabilitation Research and Development Service. Since then, he has been a rising star, also being tapped as a Career Development Scholar by the Claude D. Pepper Older Americans Independence Center in 2011.
A list of Clark’s research publications and in some cases full texts are available at this National Library of Medicine link. (Return to Archive list or Top)
Rose Receives Golden Synapse Award for Outstanding Article

Dorian K. Rose, PhD, has received the Golden Synapse award from the Academy of Neurologic Physical Therapy for an article published in the Academy’s journal. The annual award recognizes the most outstanding article of the year based on the article's conceptualization, execution, presentation, and contribution to physical therapy practice as judged by the reviewers and Editorial Board of the Journal of Neurologic Physical Therapy.
The importance of this research is that it establishes that there is an effective therapy for gait problems after stroke that is safe to start early on in rehabilitation. Such therapy is currently not done as part of standard stroke care, consequently, during the first 6 months after discharge from the hospital, there is a 73% incidence of falls among persons who have mild to moderate impairment in gait or balance or after a stroke. The therapy involves backward walking, which has several benefits, one of which is that it engages cerebral pathways that have been damaged by the stroke and thus potentially enhances neuroplastic recovery.
In addition to The Golden Synapse Award, a paper by Rose and her team in the journal, Physical Therapy, in 2017 was accompanied by an editorial in which the journal’s editor noted that the work provided “important evidence regarding dose of rehabilitation intervention following stroke.” This paper addressed the question of whether either too little or too much therapy might not help or might even hinder recovery. The article also received the University of Florida Dean’s Citation Paper Award (scroll half way down the page).
A list of Rose’s research publications and in some cases full texts are available at this National Library of Medicine link. (Return to Archive list or Top)
Waid-Ebbs Research Leads to Recommendation by Defense Health Agency for Clinical Treatment of Cognitive Dysfunction

Kay Waid-Ebbs, PhD, has succeeded on the long and winding road to the ultimate goal of health research: Definitively proving that a new, advanced treatment is safe and effective and can be used in standard care. This is particularly rewarding in that Waid-Ebbs‘s work has focused on cognitive dysfunction, a problem that perfectly illustrates the adage that little things make a big difference. In this case, even a mild brain injury can cause a big problem, for example, unpaid bills.
The Defense Health Agency (DHA) has recommended a treatment tested by Waid-Ebbs, Goal Management Training (GMT), because it “focuses on metacognitive training in goal formu¬lation, maintenance, and execution. GMT teaches patients to self-regulate by identifying errors in processing and implementing strategies to reduce these slips. The key self-regulation strategies are ‘stop, define the goal, learn the steps, and check the plan.’ (Waid-Ebbs et al., 2014).” Problems with such tasks affect many Veterans of the Gulf Wars who suffered mild as well as severe traumatic brain injury.

Although these problems may seem insignificant compared with limb loss, Dr. Waid-Ebbs noted that even minor effects on cognitive function can seriously interfere with daily activities. An interactive psychoeducational treatment, GMT involves computer-based guided presentation of information, group interaction, and practice of complex tasks. Improvement was found in an outcome measure called the Tower of London, which involves unique and complex, multi-step problems. Veterans who completed the full treatment protocol reported GMT helped them to think before engaging in a complex task, which gave time to consider implications of what they were going to do and to better plan what actions to take.
Read about the VA/DoD Clinical Practice 2021 Guidelines on Rehabilitation of Post-Acute Mild Traumatic Brain Injury.
A list of Waid-Ebb’s research articles, including the 2014 article referred to above, and in some cases full texts are available at this National Library of Medicine link. (Return to Archive list or Top)